Medicare Advantage Programs
Medicare Advantage programs generally fall into a few different types.
Here are the three most common types of Medicare Advantage programs:
Types of Medicare Advantage Programs
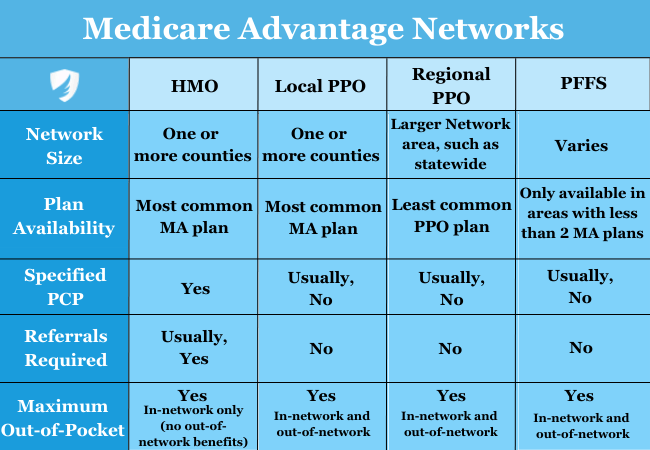
Medicare Health Maintenance Organization (HMO) plans usually require a doctor’s referral before you can see a specialist within your network. You choose a primary care doctor in your plan’s network. These plans tend to have the lowest monthly premium because they can generally be the most restrictive.
Medicare Preferred Provider Organization (PPO) plans are more flexible than HMO plans. Members can generally see doctors inside their network without a referral and receive treatment outside their network, but it will cost more.
Medicare Private Fee-For-Service (PFFS) plans do not have a network or a small network. You can see any doctor who will bill the plan as long as they accept your plan and its terms. You must ask your providers if they take the plan before you can use their service.
Other Medicare Advantage Plan Types
Special Needs Plans, or SNPs, are available only to Medicare recipients with specific health conditions or circumstances, such as being eligible for Medicaid and Medicare. These plans were created to address those particular health needs with a special provider. The majority of SNP plans are HMOs.
Medical Savings Account Plans, or MSAs, offer a health savings account along with insurance benefits. Medicare puts a set amount into your account every year, which you can spend whenever you use any qualifying health service.
Medicare Advantage Enrollment
You can pick up a Medicare Advantage plan during your seven-month Medicare Initial Enrollment Period. You can join or leave Medicare Advantage during the Medicare Open Enrollment Period (sometimes called the Annual Enrollment Period (AEP), which runs from October 15th through December 7th each year.) There is also a Medicare Advantage Open Enrollment Period, which runs from January 1st through March 31st each year. It allows individuals enrolled in a Medicare Advantage Plan to make a one-time election to go to another Medicare Advantage plan with or without prescription drug coverage to return to Original Medicare.
Multiple Special Enrollment Periods exist, and if you qualify, you may be able to join mid-year. One of the common ones is when you move to a different state and lose your existing Medicare Advantage plan. Medicare will allow you a 63-day period to choose another plan in your new state. Another Special Enrollment Period can occur if you become eligible for Medicaid or the Part D Extra Help program.



















